Although my maternal grandfather died of pancreatic cancer, I never imagined that I would lose my mother to the same illness shortly after I read the pancreatic cancer proclamation last year. But I should not have been surprised given the data demonstrating that African American families like ours have a significantly higher risk of pancreatic cancer than do White American families (1, 2). And while those differences exist, this terrible disease affects people of all walks of life including Steve Jobs, John Lewis, Alex Trebek and, as reported last week, D’Angelo (3). What may be more alarming are the data that the incidence of cancer is increasing among younger adults (4).
Scary, surprising, unfair, unbelievable were all words used to describe our responses to my mother’s diagnosis. How could a 67-year-old previously healthy woman with no chronic medical conditions, on no medications and who had less grey hair than I had be diagnosed with metastatic pancreatic cancer? We may never know the answers to those questions in my lifetime, but there is one question that I struggle to answer—if and/or when to discontinue chemotherapy.
I will never forget the day my mother decided that she wanted to transition to hospice care. After several rounds, the side effects she experienced were mounting while her quality of life (mental and physical) was declining precipitously. Following another of her unplanned post chemotherapy hospitalizations at Piedmont Fayette, I mused aloud at the kitchen table that I would not have undergone chemotherapy if I had the same cancer and would instead focus on living out the rest of my days of sound mind and in the company of those I loved. My musing seemed to be an opening for her to express that she no longer wanted to continue chemotherapy. Realizing that she was unable to recognize her own mother (in the context of an episode of temporary altered mental status) was a tipping point for her.
As a physician I knew that transitioning to hospice care was likely the best decision she could make, but as her son I still wrestle with whether I unduly influenced it. Was the exhaustion of caring for her hundreds of miles from where I lived and worked influencing how I showed up for her? Was I ready to see one of the strongest women in my life stop “fighting?” Was this truly her decision? All I know is that seeing her suffer through various states of altered mental status, nausea, weight loss and weakness that made it too difficult for her to sit upright without assistance was inconsistent with how this fiercely independent woman lived her life up until that point.
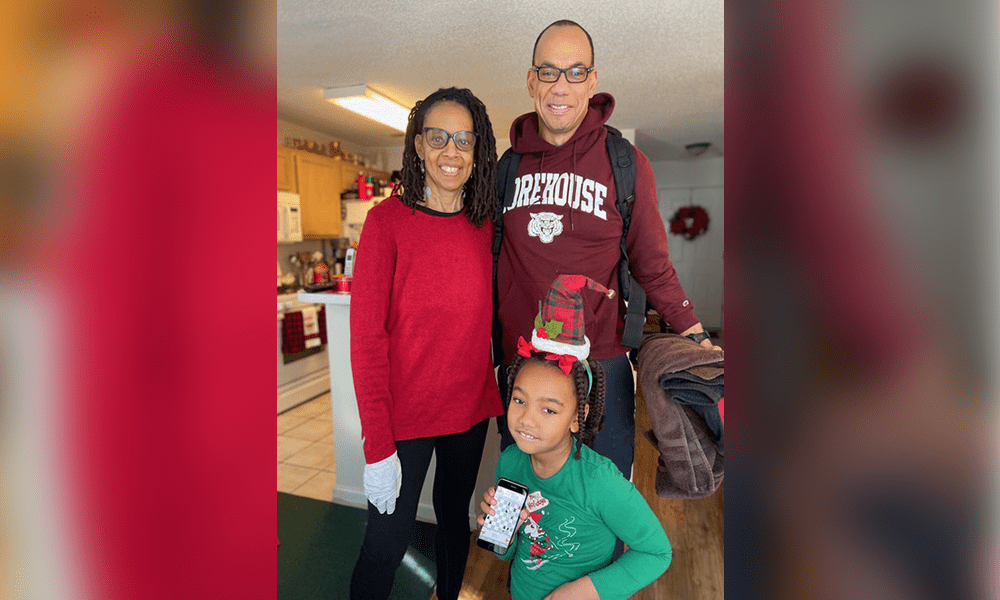
Putting aside my unease about how she arrived at her decision, I can unequivocally state that home hospice was the right choice. As she wished, she moved in with us to be in the company of her grandchildren. In fact, she took her last breath after seeing my child (her grandchild) off to school. It was as peaceful as one could have wanted—no emergency vehicles or heroic medical measures. Instead, she was surrounded by the love and comfort of family and friends. This desired end was facilitated by the comprehensive care (nursing, hospital bed, bathing/grooming, music therapy and family counselling) provided by the hospice team.
It is auspicious that November is the month to recognize pancreatic cancer and hospice/palliative care. Coincidentally, November is also the birth month of my mother—a retired Clayton County public schoolteacher. She continued teaching to the end and we followed the “lesson plan” she had for her final days. As she directed, we eschewed an open casket in favor of a celebration filled with song and joy. Dancing the famous “electric slide” in a South Fulton church sanctuary as the song “Before I Let You Go” played was a fitting sendoff for a woman who enjoyed life and danced to the beat of her own drum. And in so doing, she saved her best lesson for last—how best to transition from this life to the next.
In the end, it may be less important to determine how we arrived at the decision to transition to hospice care. What may be most important is that the best decision was made and her “plan” was followed. For that, and many more lessons, I am thankful and will be forever indebted to her and the community that helped her transition on her own terms.
References
(1) Why do Black Americans have a higher risk of pancreatic cancer than White Americans? Silverman, D. T., et. al. (2003). Epidemiology. January;14(1):45-54
(2) Pancreatic cancer disparities in African Americans. Khawja, S. N., et al. (2015). Pacreas. May;11(4):522-7.
(3) https://www.ajc.com/pulse/cancer-cases-in-younger-people-are-on-the-rise/3B3AKTFVZRDR3H36KIMR2BJ23Q/











Leave a Comment
You must be logged in to post a comment.